What is a surgical mesh for hernia repair?

- What is a surgical mesh?
- What is the history of surgical mesh?
- Characteristics of a surgical mesh
- The use of surgical mesh for hernia repairs
- What materials can a surgical mesh be made of?
- Classification of surgical meshes according to international standards
- Surgical mesh hernia repair surgery
- What are the possible complications of a surgical mesh procedure?
- Surgical meshes are made of sterile material, which allows them to be permanently implanted in the body.
- The most commonly used surgical mesh material is synthetic, although there are several types.
- Surgical mesh is commonly used for the repair of abdominal hernias.
What is a surgical mesh?
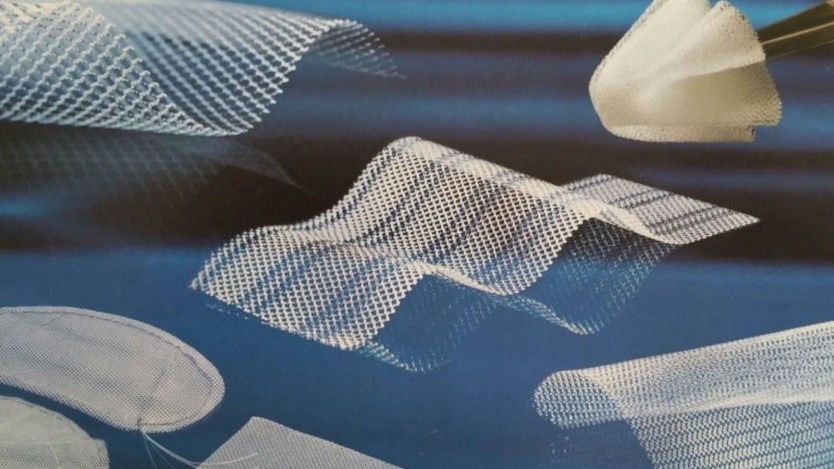
Surgical mesh is a sterile mesh material, intended to be implanted into the body, either permanently or temporarily.

Do you need inguinal hernia surgery?
Request a free and immediate appointment with our specialists
Surgical meshes have a firmness similar to that of steel, although much less density. They are stable and very durable when in contact with tissue.
It has two main functions: to reinforce areas where there are soft or weakened tissues and to act as a support point for organs and viscera that are slipping out of their anatomical structure.
Its most common application is in the repair of hernias, pelvic organ prolapse and stress urinary incontinence. In general, to reinforce tissues in different areas of the human anatomy.
The placement of the mesh in the case of a hernia keeps the viscera in place until the body itself generates tissue to keep them in place.
When a mesh is inserted into the body, the body reacts to a foreign element, often resulting in acute inflammation, which can even lead to fibrosis (pathological formation of fibrous tissue).
When a mesh is implanted, the patient may feel discomfort when moving due to the stiffness of the mesh and the formation of a scar. For this reason, lightweight meshes with larger pores are often used.

What is the history of surgical mesh?
By 1800, doctors were already beginning to realise that it was sometimes necessary to reinforce the walls of the abdomen after certain operations. But it was not until 1959 that polyethylene mesh was introduced by Francis Usher.
In 1945, Earle Shouldice theorised about mesh and developed a series of concepts that are now basic in relation to surgical mesh.
In 1948, the use of nylon mesh for hernia repair was pioneered by Acquaviva and Bourret, two surgeons of French origin.
In 1968, Dr Irving L. Lichtenstein began to perform hernia surgery using a mesh to prevent the viscera from protruding.
Characteristics of a surgical mesh
Surgical meshes can be made of absorbable material (polyglactin 910) or non-absorbable material (polyester or polypropylene fibres among others).
The meshes are usually knitted through a process that cross-links each junction of the individual fibres so that elasticity is obtained in both directions. As a result, the netting can be cut without fraying.
Characteristics common to all surgical meshes, whatever their type:
- Flexibility, to prevent chafing in other areas and to maintain their integrity.
- Porous, to promote drainage and fibre growth.
- Chemically inert, to avoid further inflammation.
In particular, hernia meshes must also incorporate the following characteristics:
- Tensile strength.
- Not deformed by body fluids.
- Do not cause allergies.
- Resist mechanical deformation.
- Suitable for the healing process and cell interaction.
The use of surgical mesh for hernia repairs
It is most widely used for hernias. When a surgical mesh is implanted for the correction of a hernia, what is done is to place the viscera that were protruding and retain them there by means of the mesh.
Depending on the patient's pathology and many other variables related to the patient and their disease, it is the doctor who must decide what type of mesh will be placed, so that the ideal mesh is placed and that it remains there permanently and does not cause complications in the future.
What materials can a surgical mesh be made of?
Depending on the origin of the materials, abdominal hernia meshes can be:
- Of biological origin: They are usually taken from the patient's own tissues, or from other patients, even from some animals.
- Of metallic origin: In the past, metals such as steel, silver or tantalum were used, combined with carbon fibres. They were no longer used because they were a factor in increasing the risk of cancer.
- Synthetic: This type of mesh remains flexible, so it does not disturb wound healing. It is used to cover and reinforce, to provide support until the wound heals.
Surgical meshes of synthetic origin are the most commonly used today and can be absorbable or non-absorbable:
- Absorbable ones are used when the abdomen is heavily contaminated and has to be closed and not reopened. In this case the mesh is used as a reinforcement that provides support during the time in which the scarring that generates the tissue that finally has to stay in place takes place. Over time and once the relevant tissue has been generated, the mesh is reabsorbed into the body itself.
- On the other hand, non-absorbable meshes must be removed once they have fulfilled their function within the patient's body. This includes mesh made of polypropylene.

Within the synthetic origin, the most commonly used materials are polypropylene and expanded polytetrafluoroethylene.
- Polypropylene mesh (PP): This is a synthetic fabric, in the shape of a net, which allows human tissue cells to intermingle with its fibres and form a resistant fabric. It is the most commonly used material for surgical meshes, especially for those used in hernias. These meshes are easily incorporated into the surrounding tissue and are highly resistant to tension and infection. A disadvantage is that this material can oxidise inside the body, reducing its strength over time, but as it is more inert and resistant to shrinkage than other materials, it is the most commonly used.
- ePTFE (expanded polytetrafluoroethylene) mesh: It is a microporous, soft and flexible mesh. The small size of its pores slows fibrous growth. It is a practically opaque material, making it more difficult to implant.
Classification of surgical meshes according to international standards
According to international standards, three types of classifications can be made:
According to pore size and behaviour during host integration
- Macroporous or reticular (type I): formed by pores larger than 75μm, usually composed of polypropylene or polyester, flexible and non-absorbable.
- Microporous or lamellar (type II): formed by pores smaller than 10-75μm, usually composed of expanded polytetrafluoroethylene, do not allow the spread of macrophages and fibroblasts, but do allow the spread of bacteria.
- Mixed (type III): They have a dual property: on their parietal side: high integration into the abdominal wall; on their visceral side: minimal excitation of the adhesive phenomenon. They are usually made of polypropylene or polyester and have an anti-adherent barrier on the visceral side.
- Organic (type IV): meshes of this type have very good tissue integration. They are not exactly meshes, as they have neither a woven weft nor pores.

Depending on the final amount of prosthetic material included within the scar
- High density. 95-110 g/m2.
- Medium density. 45-90 g/m2.
- Low density. 35-38 g/m2. Polypropylene content and large pores are reduced, leading to reduced swelling and better integration of surrounding tissues.
According to the indications for use
- Tissue or tissue interface repair without contact with the visceral peritoneum: this consists of a prosthesis that must be separated from the abdominal viscera in order to avoid adhesion. Polypropylene, polyester and polyvinylidene fluoride prostheses are usually used; the choice between one or the other must be made by the physician.
- Repair in contact with visceral peritoneum: mixed and/or expanded polytetrafluoroethylene meshes are usually used for open and laparoscopic surgery. Depending on the surgeon's choice, they may be made of polypropylene, polyester or expanded polytetrafluoroethylene.
Surgical mesh hernia repair surgery
Surgical meshes are often used to repair hernias.
First the viscera are put in place, then the mesh is put in place to make them stay in place and not move.
To implant a polypropylene mesh, it is usually necessary to use polypropylene sutures, as polypropylene mesh can react with other materials and cause the body to identify them as foreign bodies and reject them.
This material is highly resistant to acids and other chemical substances in the body.
If the mesh is non-absorbable it should be secured, as expected, with non-absorbable sutures, preferably of the same material as the mesh, or staples.

Do you need inguinal hernia surgery?
Request a free and immediate appointment with our specialists
If the mesh is absorbable, it can be secured with absorbable or non-absorbable sutures or staples.
Once the mesh is in place, it is sutured around it, taking care to do so with the correct tension. The excess mesh is then cut outside the suture and removed.
Apart from suturing, there are other ways to hold the surgical mesh in place. In the early days, this was done with staples, which were eventually adapted to the laparoscopic technique.
Surgical mesh can also be secured with pins, both permanent and absorbable, or with adhesives that are resistant to being placed inside the body.
What are the possible complications of a surgical mesh procedure?
After surgical mesh implantation, patients often experience swelling in the area due to the fluid that remains in the area after mesh insertion. Often this fluid disappears on its own, but sometimes the fluid needs to be drained.
As with any surgical procedure, infections can develop, but they are not serious and are treated with antibiotics and disappear within a few days.
Any unusual discomfort, especially in the area where the mesh has been placed, should be reported to the doctor. If you develop a fever, you should see a doctor immediately.
Medical disclaimer: All the published content in Operarme is intended to disseminate reliable medical information to the general public, and is reviewed by healthcare professionals. In any case should this information be used to perform a diagnosis, indicate a treatment, or replace the medical assessment of a professional in a face to face consultation. Find more information in the links below:
