Transurethral resection of the prostate (TURP)

- What do we know about the prostate?
- What are the most common diseases that commonly affect the prostate?
- What is transurethral resection of the prostate?
- When is transurethral resection of the prostate indicated compared to open or laparoscopic surgery?
- What are the most common complications of transurethral resection of the prostate?
- What are the alternatives to transurethral resection of the prostate?
What do we know about the prostate?
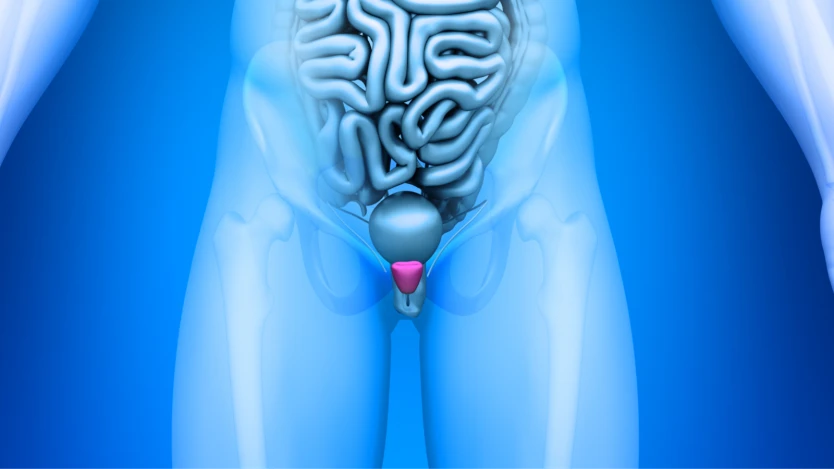
The prostate is a gland found exclusively in the genital and urinary tract of the male sex. It is made up of tissue with a glandular function and tissues with a muscular function that serve to give it a certain capacity for contraction. It weighs approximately 20 grams.

Do you need prostate surgery?
Request a free and immediate appointment with our specialists in Urology
From the point of view of its location in the human body, the prostate is located in front of the colon, more specifically in front of the end of the colon, known as the rectum, around the neck of the bladder (a funnel-shaped structure capable of filling with urine) and the urethra (a duct that leaves the bladder and communicates with the exterior through the penis, serving as a channel for the excretion of urine).
The main function of the prostate is to synthesise, together with the glands around the urethra and the seminal glands, seminal fluid.

The shape of the prostate is classically considered to be comparable to that of a chestnut; it has a hard consistency, although with a certain elastic component, and can only be palpated by means of a rectal examination. This diagnostic manoeuvre can only be used to palpate the posterior part of the prostate.
What are the most common diseases that commonly affect the prostate?
The most common prostate diseases today are usually divided into prostatitis, benign prostatic hyperplasia and prostate cancer. Prostatitis is, as the name suggests, an inflammation of the prostate gland. It can be of infectious or non-infectious origin and can be chronic or acute.
This type of pathology usually has clinical symptoms similar to those of a urinary tract infection or cystitis (dysuria or burning discomfort during urination, pollakiuria, increased frequency of urination compared to the usual rhythm of each patient and urgency, the sensation of having to urinate just after having finished urinating).
When the origin of this prostate inflammation is infectious, it is usually necessary to use antibiotics that have a preference for action by prostate tissue (a specific type of antibiotic such as some quinolones is the most frequently used), the duration of treatment is usually extensive in time, lasting up to several weeks.
Benign prostatic hypertrophy or also called prostatic adenoma is a proliferation of the glandular tissue that forms part of the prostate with benign characteristics but which can lead to a large number of complications and morbidity that make the day-to-day life of patients who suffer from it very difficult: a decrease in urine calibre, inability to completely empty the bladder after each urination, an increase in the frequency of urinary infection, acute urine retention if the compression exerted by the prostate on the urethra is such that it completely blocks the passage of urine and, ultimately, renal failure or worsening of the patients' renal function with the consequent renal damage.

The frequency of BPH is difficult to obtain with certainty as it is a disease whose heterogeneous clinical pattern leads to a high rate of under-diagnosis. However, we can say for certain that BPH is one of the most prevalent benign neoplasms in men and that it is directly related to age (the older the patient, the more likely he is to suffer from BPH).
It is estimated that BPH is found in 0.75% of cases in patients aged between 40-60 years, in patients over 50 years the prevalence increases to 11% and in patients over 70 years it is around 30% of patients.
Prostate cancer is another of the pathologies which, due to its frequency, should be taken into account when talking about the prostate. According to the latest studies, it seems that prostate cancer is a cancer which evolves slowly and that in the vast majority of cases it is not aggressive enough to cause major complications. In a smaller number of cases, however, it does evolve rapidly and can cause, among other complications, the death of the patients who suffer from it.
The diagnosis is made by taking a biopsy of the prostate, usually by means of or guided by transrectal ultrasound. The treatment of this pathology differs greatly from patient to patient and it is vitally important to individualise each therapeutic action.
In general, we can choose to initiate treatment, almost always curative, with radiotherapy, surgical treatment and hormonal and chemotherapy treatment.

Do you need prostate surgery?
Request a free and immediate appointment with our specialists in Urology
What is transurethral resection of the prostate?
Transurethral resection of the prostate (TURP) is an operation of intermediate difficulty that consists of the introduction of an apparatus called a resectoscope through the urethra, which is the tube that runs from the tip of the penis and through it to the bladder.
This device, called a resectoscope, is shaped like a tube, measures no more than a few millimetres and, by means of a camera attached to its initial end, allows the path along which the resectoscope is introduced to be visualised.
Once the location of the prostate has been reached, instruments can be introduced through the resectoscope to fractionate the prostate from the inside and extract it through the same device, thereby reducing the size of the prostate or even removing it completely.
Transurethral resection of the prostate (TURP) is usually performed under epidural anaesthesia. TURP is initiated when the patient arrives in the operating room and the anaesthesiologist infiltrates anaesthetic medication into the epidural space of the patient's spine (the space above some of the layers of the spinal cord and which carries cerebrospinal fluid within it).
This infiltration is usually painless and quickly ensures that the patient has no sensation from the middle of the abdomen to the legs, allowing the surgeon to work comfortably and eliminating all the complications that can arise from general anaesthesia. During the entire transurethral resection of the prostate (TURP) surgery, the patient will never feel pain or discomfort.
Generally, the postoperative period after transurethral resection of the prostate is around 4-7 days, during which it is usually necessary to use a bladder catheter to ensure that urinary flow remains stable after the surgery.
When is transurethral resection of the prostate indicated compared to open or laparoscopic surgery?
The usual form of presentation of benign prostatic hyperplasia is the presence of urinary obstructive signs such as decreased urinary flow, urinary retention, urinary leakage, increased infections.
At this point it is necessary to perform a rectal examination and check for enlargement using prostate ultrasound.
This fundamental test for prostate pathology will calculate the approximate size and weight of the prostate gland.
If the prostate is between 30 and 60 grams, the technique of choice is transurethral resection of the prostate. If the prostate is larger than 60 grams, surgery is generally indicated, either using laparoscopic or open surgery or laser techniques, such as the holmium laser.
The procedure of transurethral resection of the prostate has been scientifically proven to produce great relief of urinary flow obstruction and to significantly improve the quality of life of patients suffering from obstruction of the urinary tract due to an enlarged prostate.

Do you need TURP prostate surgery?
Request a free and immediate appointment with our specialists in Urology
What are the most common complications of transurethral resection of the prostate?
Perioperative complications related to prostate manipulation are rare, the most frequent being the need for blood transfusion (0.4-7.1%), urinary retention (3-9%), urinary tract infections (1.7-8.2%) and clot retention (2-5%).
Retrograde ejaculation may occur in the days or months following the surgical procedure, although the numbers of complications are gradually improving.
What are the alternatives to transurethral resection of the prostate?
Depending on the size of the prostate gland, other alternatives to transurethral resection of the prostate have been developed in recent times and are becoming increasingly important in the treatment of benign prostatic hyperplasia.
This type of intervention is laser-mediated intervention, among which there are 3 large groups such as the green laser, the Tullium laser and the Holmium laser.
The main advantage of this type of intervention is that it minimises the rate of complications derived from prostatectomy and transurethral resection of the prostate and reduces the time spent in hospital after the intervention and the maintenance of the bladder catheter to 24 hours.

The operation of this type of intervention can be summarised in that the laser, depending on its type, emits a series of particles called photons that are capable of transmitting their energy to the tissue cells that are close to them.
This energy can cause the cells to heat the water that is housed inside them (we would have a vaporisation effect), or they can burn, achieving a photo-thermal effect.
This process depends on the exposure time of the laser on the tissue, it will also depend on whether the exposure to the laser is continuous or in bursts and finally, on the temperature that the cells reach when in contact with the laser. By way of example, we could say that at 100ºC the water inside the cells evaporates and at over 100ºC the organic compounds are volatilised.
Within all these types of laser interventions we could classify them according to the size of the prostate:
- GreenLight laser: this is currently an older type of laser than the modern Tulium and Holmium lasers, although it was one of the first to be used with the prostate vaporisation system mentioned above. Its use is recommended for the prostate <50 grams.
- Thulium laser is a great alternative for small prostates (<30g) and medium sized prostates (30-60 grams), it is perfectly compatible with patients taking anticoagulant medication and is an alternative to be taken into account in patients with enlarged prostates who present risk factors.
- Holmium laser: this is an alternative for small, medium and large prostates in patients with/without added risk factors. With this technique it is possible to perform two types of intervention: vaporisation and enucleation.
Another current alternative is the urethral release prostate surgery with the Urolift system. This is an operation in which by placing implants on both sides of the prostate attached to natural elements, an increase in the calibre of the urethra is achieved by compressing the prostate gland on both sides of the urethra, thereby improving the clinical symptoms caused by benign prostatic hyperplasia.
It is recommended for use in prostates of 50 grams or less.
The surgery is performed on an outpatient basis and full recovery is within 2 weeks. Surprisingly, in many cases the patient notices improvements in urination on the same day.
Medical disclaimer: All the published content in Operarme is intended to disseminate reliable medical information to the general public, and is reviewed by healthcare professionals. In any case should this information be used to perform a diagnosis, indicate a treatment, or replace the medical assessment of a professional in a face to face consultation. Find more information in the links below:
