Haemorrhoids: what they are, causes, symptoms and treatment

- What are haemorrhoids?
- Why do haemorrhoids occur?
- Risk factors for the onset of haemorrhoids
- How to prevent haemorrhoids?
- Symptoms of haemorrhoids
- Types of haemorrhoids
- Complications of haemorrhoids
- Conservative treatment for haemorrhoids
- Surgical treatment of haemorrhoids
- Haemorrhoids are one of the most common medical problems of the anal canal today due to poor diet and a sedentary lifestyle.
- It is estimated that about 80% of the population will suffer some episode of haemorrhoids in their lifetime.
- In the most severe cases of haemorrhoids, the only definitive solution is surgery. Here we explain everything you need to know about haemorrhoids.
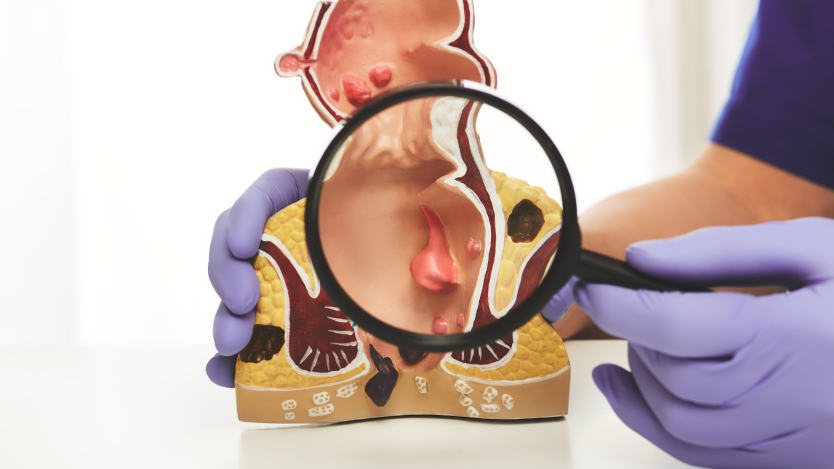
What are haemorrhoids?
Haemorrhoids consist of varicose dilation of the veins that form the haemorrhoidal plexus, located in the lower part of the anal canal.
This dilatation is of the same type as varicose veins in the legs or varicocele, although in this case, as it affects the haemorrhoidal veins, it receives this name.

Do you need assessment from a general surgeon?
Purchase your medical voucher easily under Operarme's guarantees and attend a private consultation with a proctologist.
Depending on the severity of the haemorrhoids, they may protrude outwards, remain there, hurt a lot or a little when passing stools, bleed or even cause discomfort when walking, sitting or standing for long periods of time.
Their incidence is usually higher in men than in women, especially in those over 40 years of age, although many women suffer from them in the pregnancy and postpartum period.
Haemorrhoids, often referred to as piles, are a common problem but do not always have to be serious.
In fact, in most cases they are temporary discomforts that can be prevented or solved by drinking plenty of water, eating a balanced diet rich in fibre and exercising.
We have all noticed itching or stinging in the area, and even a little bleeding at some point (if it is continuous or very frequent, it is advisable to see a specialist in general surgery and the digestive system), but these cases of haemorrhoids are mild and cannot be compared with the severe cases we will describe below.
Mild cases can be treated with behavioural changes and even with the use of ointment and ointments, as well as sitz baths, while in severe cases (grades 3 and 4, which we will explain below) the only definitive solution is surgery to remove the haemorrhoids.
Why do haemorrhoids occur?
The haemorrhoidal plexuses, in addition to the blood vessels that eventually become haemorrhoids, are also made up of smooth muscle and connective tissue that help expel stool and maintain continence.
Over time, as people get older, the muscle tissue that holds the blood vessels in place loses strength and little by little the veins become slippery, bleeding and even bulging, forming what we all know as haemorrhoids.
Risk factors for the onset of haemorrhoids
We are going to list the risk factors for suffering from haemorrhoids. It should be borne in mind that meeting any one of them does not mean that haemorrhoids will appear, as there are usually several factors that influence this:
Hereditary factors
In people whose families have a history of people with haemorrhoids, the chances of suffering from haemorrhoids are greater than in others. Therefore, in these cases it is important to lead an active life, eat a balanced diet and avoid a sedentary lifestyle.
Undesirable lifestyle habits
There are a number of dietary and day-to-day behaviours that many of us follow that can encourage the formation of haemorrhoids. These are:
- Sedentary lifestyle: This is probably one of the most determining factors. Spending long periods of time sitting without exercise (remember that exercise promotes blood flow and intestinal transit) greatly favours the formation of haemorrhoids.
- Standing: Just as sitting in the same position for a long time is bad, so is standing in the same position.
- Bad defecation habits: Spending a lot of time sitting on the toilet or exerting a lot of pressure when defecating, promote inflammation of the haemorrhoidal plexuses. Similarly, the way we defecate is not strictly natural according to some sources (it should be squatting), although this is difficult to change at this stage.
- Pregnancy: As with overweight, pregnancy puts additional pressure on the rectum that can favour the appearance of the dreaded haemorrhoids.
- Associated diseases: Hypertension, circulatory problems, inflammatory bowel diseases, etc. can also contribute to varicose dilatation of the haemorrhoidal plexuses.
- Smoking: Smoking is not good, but in this case we refer to it as a cause of deficiencies in blood circulation, which favours the appearance of varicose veins, both in the legs and in the veins that make up the final portion of the anal canal.
Poor diet
This is one of the most important aspects, as a diet poor in fibre causes excessive straining during defecation and can affect the haemorrhoidal plexuses:
- Obesity/overweight: As with pregnancy, being overweight puts continuous pressure on the anal canal, which, as you can imagine, leads to dilation of the haemorrhoidal veins and consequent haemorrhoids.
- Low fibre: A poorly balanced diet with a lack of vegetables and fruit (the main source of fibre) leads to problems such as constipation and hardening of the stool. All this, as we have already mentioned, only increases the chances of suffering from the annoying haemorrhoids.
- Not recommended foods: These are not direct causes, like almost none of the factors mentioned above, but excessive consumption of alcohol, coffee, salt and spicy foods that irritate the anal area can be key factors in the formation of haemorrhoids.
Other factors
There are other factors that can favour the appearance of haemorrhoids:
- Anal sex: Anal sex without proper lubrication and care on a regular basis can cause dilation and inflammation of the haemorrhoidal plexus in the area and even cause an anal fissure, which causes a lot of pain and usually requires surgery in most cases.
- Diarrhoea: Just as suffering from constipation can favour the appearance of haemorrhoids, persistent diarrhoea can also help them to appear, due to the irritation suffered by the anal canal during this type of bowel movement.
How to prevent haemorrhoids?
Regardless of whether a person has a genetic predisposition to suffer from haemorrhoids, the best way to prevent haemorrhoids is to lead an active life and eat a balanced diet:
- Do at least 1 hour of exercise a day: This can consist of walking for an hour, which we can all do by running a few errands or going for a stroll. It is also advisable not to spend many hours sitting in a chair, but to get up from time to time, not only to avoid haemorrhoids but also back problems and so on.
- Eating a diet rich in fibre: A balanced diet rich in fibre promotes intestinal transit, reduces the chances of constipation and, therefore, reduces the chances of the annoying haemorrhoids appearing.
- Drink plenty of water: Drinking plenty of water, but not too much (2 litres a day is fine if you do not do much sport), helps stool softening and blood circulation, so it is all good for preventing haemorrhoids.
- Spend little time sitting when defecating: If we lead an active life, eat a diet rich in fibre and drink plenty of fluids, intestinal transit is much easier and more fluid, so it is easy to spend little time sitting when going to the toilet. On the other hand, if none of these aspects are met, it is normal to spend more time sitting down and, as a result, the formation of haemorrhoids is encouraged.

In conclusion, leading an active and healthy life is the best option to avoid the appearance of haemorrhoids. However, it is still possible for this pathology to occur, so we will proceed to indicate the symptoms and other relevant aspects related to what are popularly known as piles.
Symptoms of haemorrhoids
Although the main symptom of haemorrhoids is bleeding, it also occurs in other pathologies of the anal canal such as fissures. Here we explain the different symptoms that haemorrhoids can cause:
- Bleeding: It is common to detect red blood on toilet paper in the early stages of the problem. The difference between detecting red blood and darker, pasty-textured blood is that darker blood indicates that the haemorrhoids have been present for longer and are higher up in the anal canal. This indicates that the haemorrhoids are chronic and may eventually require surgery.
- Itching and heaviness in the area: In chronic haemorrhoids, the patient notices continuous itching and heaviness in the area, especially when sitting. This is one of the most annoying symptoms.
- Pain: Pain as such appears when the pathology is very advanced (grades 3 and 4) and the affected haemorrhoidal plexuses are trapped on the outside by the sphincter. This problem can lead to complications such as thrombosed haemorrhoids and must be solved by a medical professional.
Types of haemorrhoids
Haemorrhoids can be classified according to their severity and surgical indication. Haemorrhoids susceptible to surgery are internal haemorrhoids that prolapse to the outside and become trapped.
The rest can be treated conservatively to prevent them from worsening and requiring surgery:
- Grade 1 haemorrhoids: In this case, the haemorrhoids remain inside the anal canal during defecation without prolapsing to the outside. A small amount of blood may be felt during defecation.
- Grade 2 haemorrhoids: In this case, the haemorrhoids are eventually protruded during bowel movements, but spontaneously return to the inside of the anal canal. Bleeding, itching or heaviness is usually felt here, at least at certain times.
- Grade 3 haemorrhoids: This is one of the most serious cases, as the haemorrhoids prolapse to the outside and become trapped outside, without returning spontaneously. In these cases the patient is able to reintroduce them by hand or by using a bit of toilet paper. Pain is more common in these stages of the problem.
- Grade 4 haemorrhoids: This is the most serious case of haemorrhoids and the one that is most commonly operated on due to the severe discomfort it causes in the patient's daily life. The haemorrhoids prolapse outwards, become trapped by the sphincter and cannot be reduced manually by the patient, but must be reduced by a medical professional and may even require emergency surgery due to complications. The best thing to do in these cases is for the patient to schedule surgery and eliminate the problem permanently.

These last two degrees of haemorrhoids are the ones that cause the most discomfort to patients who suffer from them and the ones that are usually indicated for surgery.
If the patient suffers from this type of problem and is considering a definitive solution with surgery, the best option is to consult a specialist in General and Digestive System Surgery.
Complications of haemorrhoids
The complications of haemorrhoids tend to be mainly related to level 4 of severity of the pathology, as this is when the plexus is on the outside, suffers more contact and friction, and also loses blood supply due to the pressure exerted by the sphincter.
These complications are:
- Bleeding haemorrhoids: While haemorrhoids cause bleeding on a regular basis, in this case we mean that the haemorrhoids trapped on the outside are dried out and in continuous contact with the patient's underwear. This, together with defecation, can cause small fissures in the veins and cause significant bleeding. It is usually felt when wiping after defecation and if this is prolonged over time it can lead to anaemia.
- Thrombosed haemorrhoids: When the haemorrhoidal plexus is trapped on the outside by the sphincter, the blood supply is reduced and the haemorrhoids may turn a dark purplish colour. The main symptom is continuous sharp pain and is often an aggravation of bleeding haemorrhoids. At this point, if it has not been decided to solve it definitively with surgery before, it is important to consider it seriously as the discomfort is tremendous.
Conservative treatment for haemorrhoids
Patients who suffer from haemorrhoids, but are not serious enough to require surgical intervention, can benefit from conservative treatment to solve their problem.
The best option when faced with haemorrhoids is always prevention, although the same points that allow us to avoid them can help us to solve mild cases.
Below we explain some points that may be of interest:
- A balanced diet rich in fibre: As we mentioned in the prevention section, eating a diet rich in fruit and vegetables helps with intestinal transit, which favours the evacuation of faeces and minimises the strain on the haemorrhoidal veins.
- Drink plenty of fluids: This helps with defecation, avoiding overexertion of the haemorrhoids.
- Avoid toilet paper: Use wet wipes for cleaning after bowel movements, avoiding rubbing the haemorrhoids.
- Sitz baths: In a bidet with lukewarm water three times a day or in the shower. It is also advisable to do this after going to the toilet.
- Maintain an active lifestyle: Promoting blood circulation and intestinal transit.
- Use a haemorrhoidal pad: To avoid putting pressure on the anus when sitting. This is more of a symptom reliever than a solution. It is a cushion with a hole in the centre.
- Ointments: There are some ointments that can help the patient to reduce the symptoms and inflammation of haemorrhoids in acute cases.

Despite this advice, many cases cannot be solved conservatively and the best option is to eliminate the problem permanently with haemorrhoid surgery.
This is a simple operation (performed by a specialist, of course), very common and with excellent results. Below we explain step by step what haemorrhoid surgery consists of.
Surgical treatment of haemorrhoids
Once the patient has seen a specialist in General and Digestive Surgery and it has been decided to carry out the haemorrhoid surgery, it will be necessary to carry out a complete preoperative examination to determine the type of anaesthesia required for the patient and whether there is any problem that would contraindicate the surgery.
The preoperative period for haemorrhoid surgery, and for practically any surgery, consists of 3 tests:
- Electrocardiogram: The electrocardiogram provides information about the health of the patient's heart and whether he or she is able to cope with the operation. In principle, there are usually no problems.
- Complete blood test: This test checks for signs of infection that could cause problems. If so, the infection will need to be checked before surgery.
- Chest X-ray: This test is only performed if the doctor considers it appropriate, and allows us to know if the trachea is well positioned and if there is infection or not.
Once the pre-operative procedure has been carried out, the patient will go to an anaesthesia consultation where it will be determined whether he/she is fit and what type of anaesthesia will be required. If the anaesthesiologist gives the go-ahead, the only thing left to do is to perform the operation on the appointed day.
On arrival at the hospital on the agreed day, the patient hands in the necessary documentation at the admission desk and is then escorted to a waiting room where he or she will be called to the operating theatre in a few minutes.

First of all, you will be asked to undress in the pre-surgical room and to put on your surgical clothes for the operation.
Afterwards, you will be taken to the operating theatre, where the specialist in General and Digestive Surgery, the anaesthetist and one or two members of the nursing team will assist in the surgery.
The anaesthesia will be administered, which is usually regional with sedation, although in some cases general anaesthesia may be required; and when it takes effect, the surgery will begin:
- Haemorrhoid surgery is performed by means of a haemorrhoidectomy, which can be open or closed, with the only difference being that in closed haemorrhoid surgery a suture is used and in closed haemorrhoid surgery it is not. This is at the surgeon's discretion in each case.
- First, the surgeon dilates the anal canal and extracts the vascular plexus of haemorrhoidal veins from the inside using surgical forceps.
- Thanks to this dilation, the specialist can see the origin of the haemorrhoids and access the highest part where they are located, where the haemorrhoidal plexus will be sectioned and the problem removed.
- In the case of laser surgery, the process is the same, except that the section is performed with a CO2 laser, which reduces bleeding during the cut, which in any case is not very high.
- Once all the affected veins have been removed, the surgeon makes sure that there are no problems and the operation is finished.
After the surgical intervention, the patient is woken up and taken to a recovery room where he or she will finish recovering from the anaesthesia.
Haemorrhoid surgery lasts between 90 and 120 minutes, depending on each case.
The hospital stay is approximately one night, although sometimes patients can leave the same day.
Full recovery is achieved after 10 to 15 days.

Do you need laser haemorrhoids surgery?
Request a free and immediate appointment with our specialists in general surgery
Medical disclaimer: All the published content in Operarme is intended to disseminate reliable medical information to the general public, and is reviewed by healthcare professionals. In any case should this information be used to perform a diagnosis, indicate a treatment, or replace the medical assessment of a professional in a face to face consultation. Find more information in the links below:



